Gastrointestinal problems are among the most common symptoms of stress. Have you ever felt a knot in your stomach during a tense meeting? Or needed an urgent trip to the toilet after an argument? That’s the brain-gut connection at work — a powerful biological relationship between stress and your digestive system.
Common Stress-Related Digestive Issues
Stress can significantly affect how your digestive system works. Some of the most common digestive issues linked to stress include:
- Diarrhea
- Constipation
- Stomach cramps and aches
- Lower abdominal pain
- Indigestion
- Changes in appetite
- Nausea
- Irritable Bowel Syndrome (IBS)
- Peptic ulcers
The Brain-Gut Connection Explained
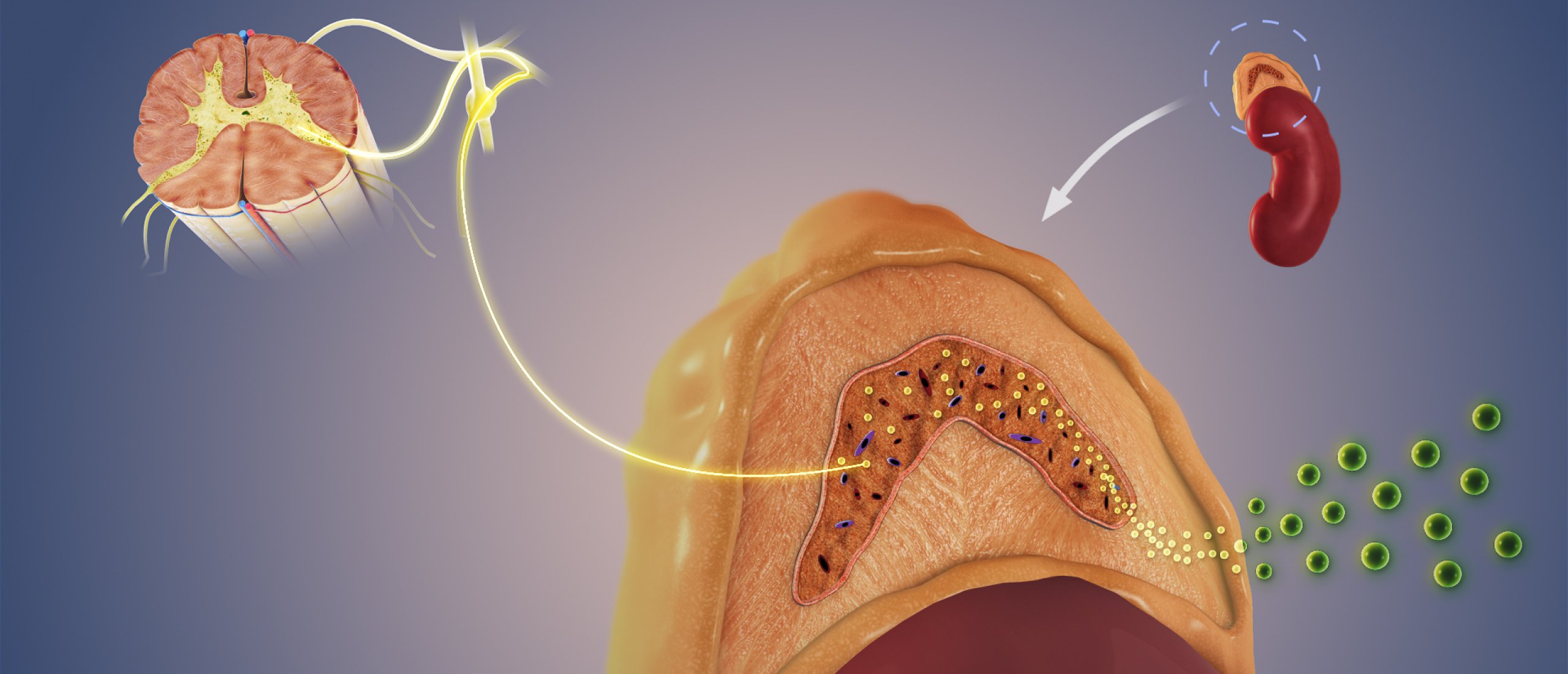
The gut contains the largest number of neurons outside the brain and is sometimes called the "second brain" — officially known as the enteric nervous system. This system communicates directly with the brain via the vagus nerve, forming the basis of the gut-brain axis.
Both the sympathetic and parasympathetic nervous systems regulate this communication. The sympathetic system drives the stress response, while the parasympathetic system helps calm things down. That’s why practices like breathing exercises that activate the parasympathetic system can help reduce digestive symptoms caused by stress.
How Stress Alters Gut Function
Stress changes the motility of your digestive tract:
- Upper gut: Reduced movement, slowing digestion. May trigger nausea or appetite loss.
- Lower gut: Increased activity, leading to faster stool transit and diarrhea.
These reactions are likely evolutionary defenses — limiting food intake and eliminating threats more rapidly during stress.
The Role of CRF in Digestive Stress
Corticotropin-releasing factor (CRF) is a key hormone released by the hypothalamus during stress. CRF stimulates:
- The locus coeruleus (a brain region involved in arousal and alertness)
- The adrenal glands, producing adrenaline and cortisol
CRF can also be released locally in the gut, where it activates mast cells. These immune cells release molecules that cause inflammation and increase gut motility — leading to diarrhea, pain, or cramping.
Brain Regions That Drive Digestive Stress
- Amygdala: Triggers fear and activates stress responses.
- Hypothalamus: Releases CRF to initiate hormonal stress response.
- Locus coeruleus: Produces noradrenaline and reinforces stress circuits.
These regions create a feedback loop that intensifies stress and impacts gastrointestinal function.
Stress, Digestive Disorders, and Disease
Irritable Bowel Syndrome (IBS)
IBS symptoms like cramps, diarrhea, and bloating worsen under stress. Patients with IBS show exaggerated responses to CRF, making their digestive systems highly sensitive.
Dyspepsia (Indigestion)
This condition is linked to delayed stomach emptying. Stress makes symptoms more likely and more severe.
Peptic Ulcers
While once blamed solely on stress, ulcers are now known to involve dopamine and possibly cortisol. Lower dopamine activity during stress — as seen in Parkinson’s patients — may contribute to ulcer formation.
Inflammatory Bowel Disease (IBD)
Stress is a known trigger in Crohn’s disease and ulcerative colitis, although the precise causal relationship is unclear. Research points to CRF and immune system imbalance as possible links.
Gut Microbiota: The Missing Piece in the Stress Puzzle
The bacteria in your gut (microbiota) play a surprising role in your emotional and digestive health. They:
- Influence brain function and development
- Communicate with the brain via the vagus nerve and immune signals
- Are affected by — and can affect — stress responses
Chronic stress disrupts microbiota balance, which may make you more stress-sensitive. Conversely, healthy gut bacteria reduce stress sensitivity and related symptoms.
Reducing Digestive Issues Through Stress Management
1. Support a Healthy Microbiota
Eat a diet rich in vegetables, fruits, and fiber. This nourishes "good" bacteria and restores balance.
2. Use Psychological Techniques
- Mind-body approaches: Breathing exercises, yoga, meditation
- Psychotherapy or hypnosis: Especially helpful for IBS or dyspepsia
- Antidepressants (low dose): Can reduce brain sensitivity to gut pain
3. Focus on Prevention
Managing stress can help prevent digestive flare-ups. That includes addressing root causes of chronic stress and improving resilience.
Understanding how closely linked stress and digestive issues are empowers you to take control of your health. At Stressinsight, we offer science-backed strategies to help you manage stress, improve gut health, and enhance your overall well-being.